How Is Each Part of Medicare Funded?
Find Cheap Medicare Plans in Your Area
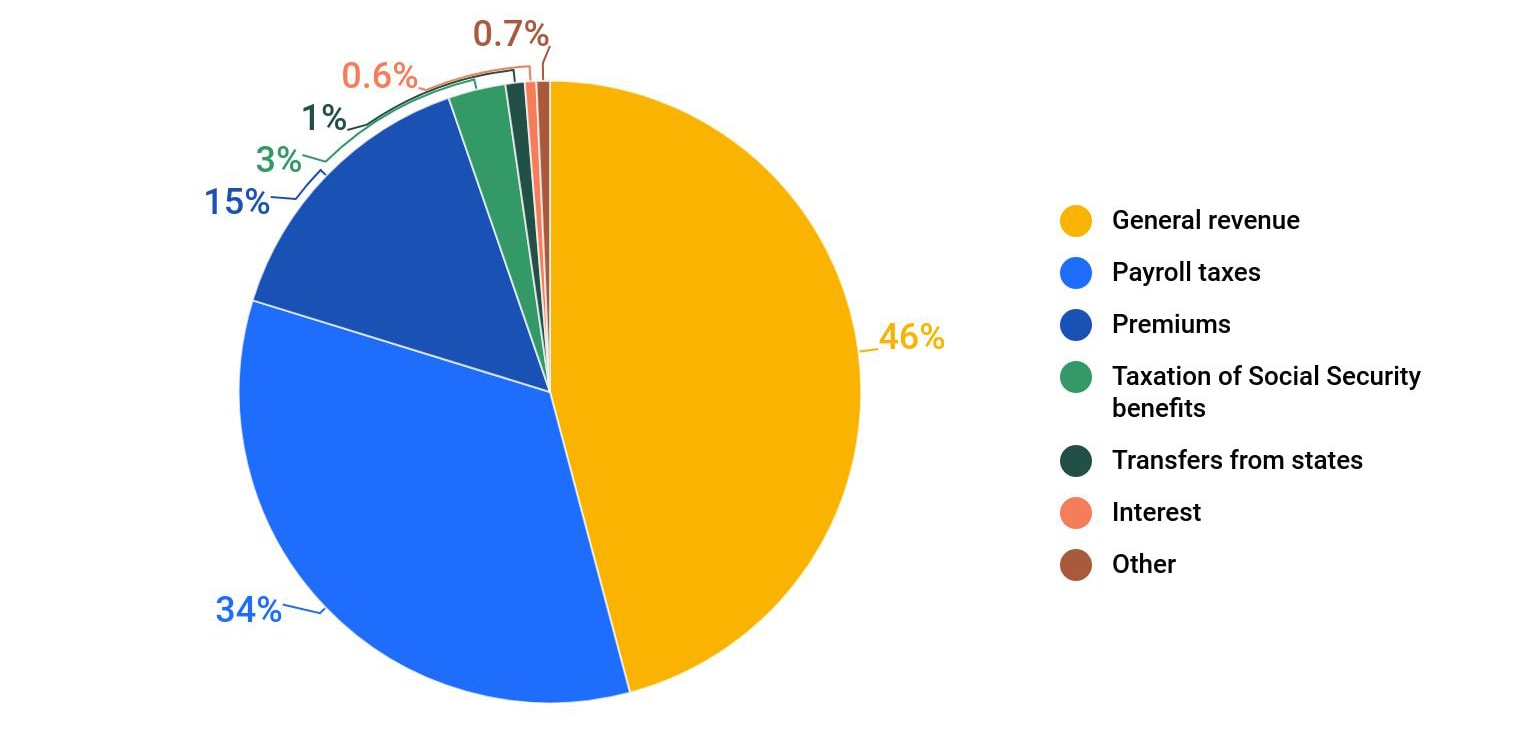
The Medicare program is primarily funded through a combination of payroll taxes, general revenues and premiums paid by beneficiaries. Other sources of revenues include taxes on Social Security benefits, payments from states and interest on payments and investments.
Overview of Medicare funding
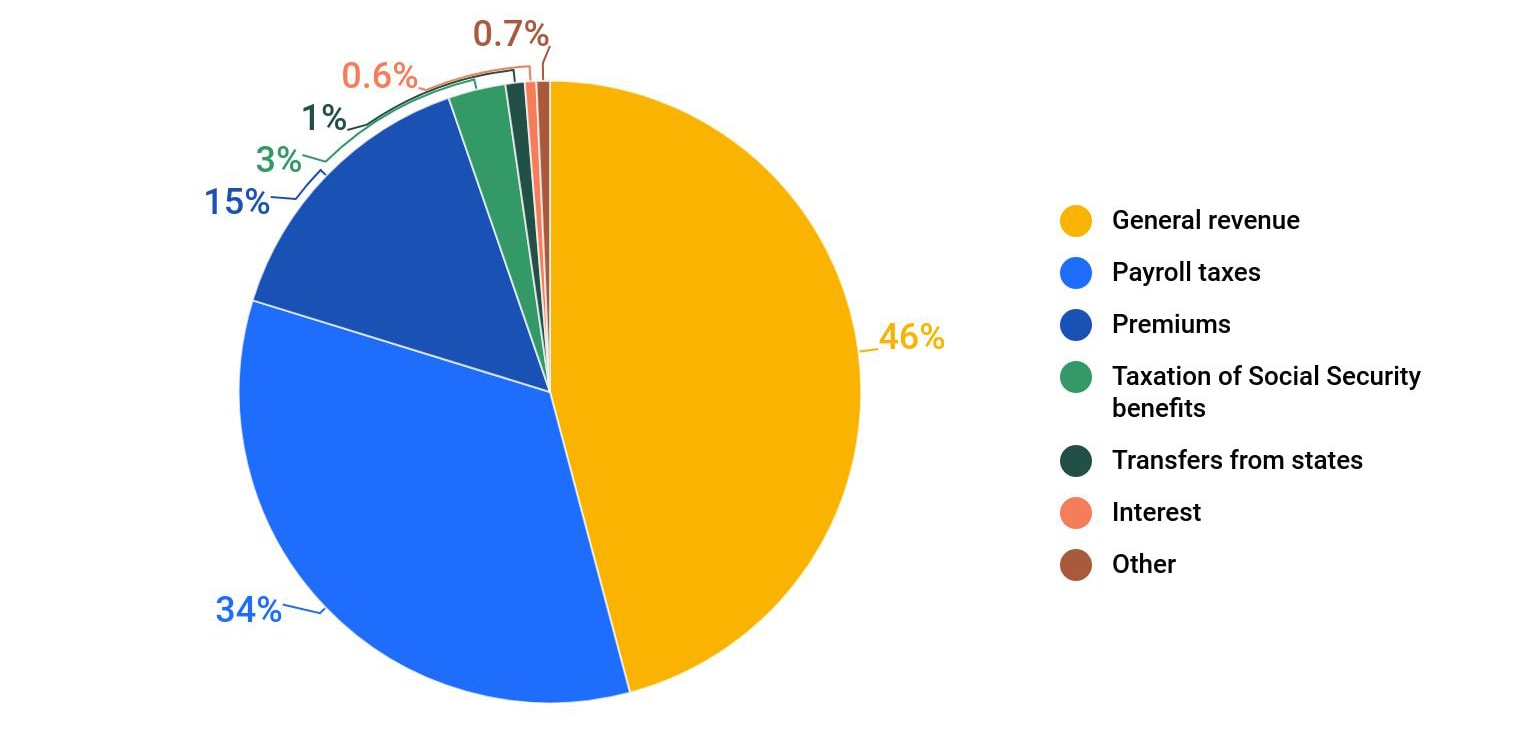
The disparate parts of Medicare are funded in different ways. Medicare Part A, which covers hospital and inpatient care, receives most of its funding, 89%, from payroll taxes.
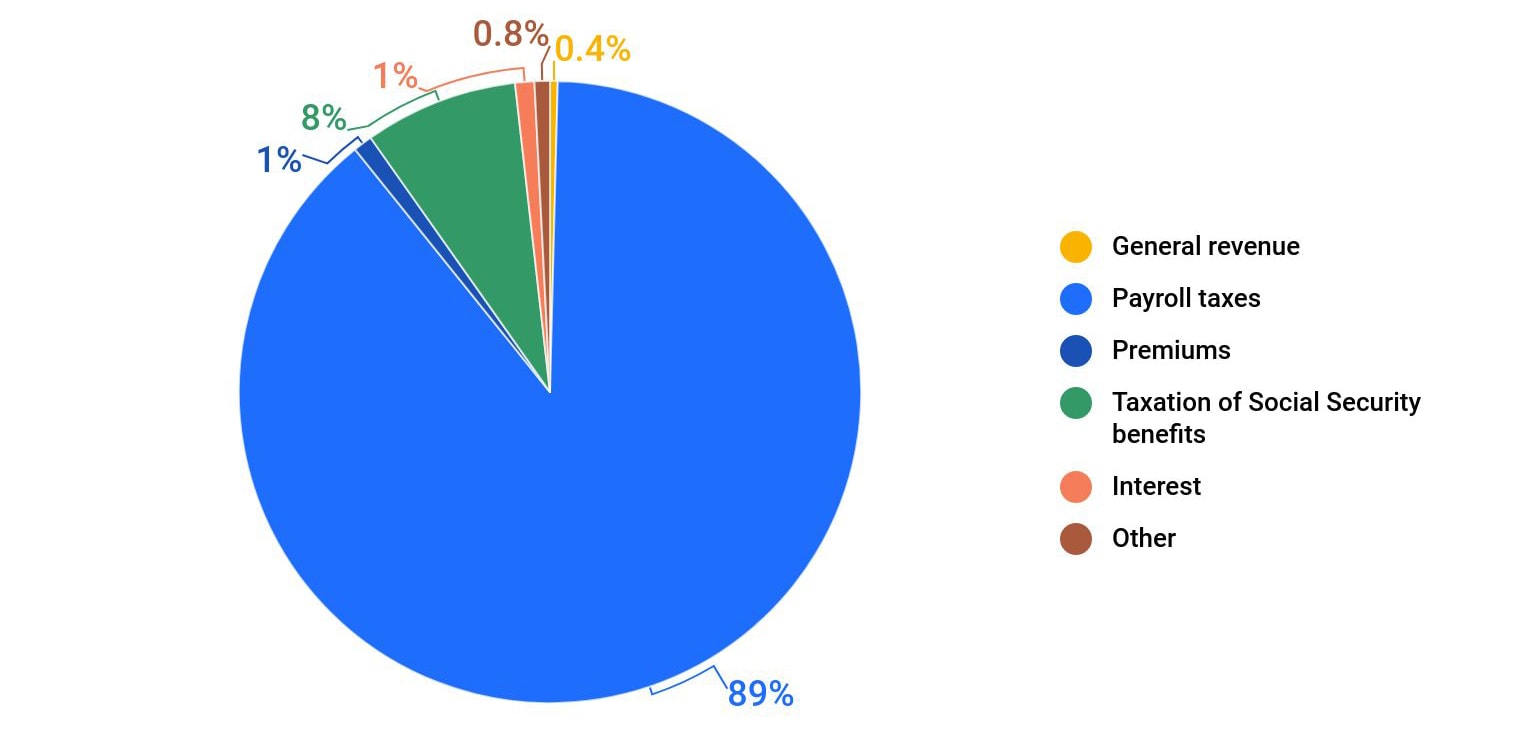
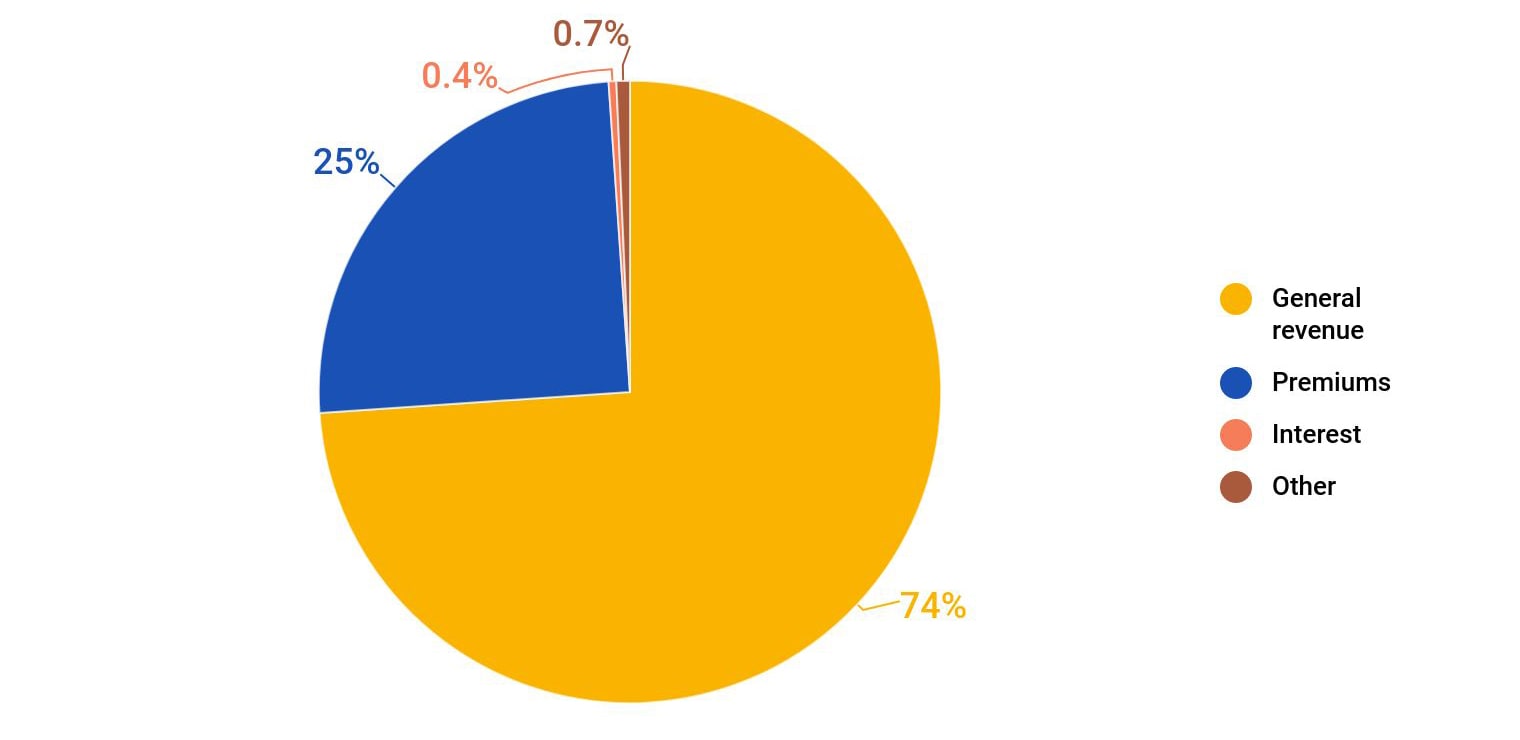
Medicare Part B, which covers outpatient services, obtains most of its funding, 74%, from general revenue. General revenue is money taken in by the federal government from taxes and nontax sources to fund government programs. Medicare Part D, an optional benefit that covers prescription drug costs, also receives most of its funding, 73%, from general revenue.
Medicare Part C — also known as Medicare Advantage — is funded by Medicare Parts A, B and D as well as monthly premiums enrollees pay for their plan. A Medicare Advantage plan is an alternative to Original Medicare that enables the beneficiary to receive a bundle of Medicare coverage through a private health insurance plan.
How is Medicare funded?
Overall
Part A
Part B
Part D
Overall
Part A
Part B
Part D
Find Cheap Medicare Plans in Your Area
How is Medicare Part A funded?
Medicare Part A derives most of its funding from a payroll tax of 2.9% on earnings, with employers and employees each paying 1.45%.
High-income earners pay a slightly higher percentage, and the self-employed pay the full 2.9% tax with their quarterly filings.
All workers in the United States are required to pay the tax on their wages, and the tax itself is grouped under the Federal Insurance Contributions Act (FICA). The tax, also known as the Medicare tax, is deducted automatically as part of the payroll process.
Medicare Part A spent $341.7 billion in 2020, the majority of funds — 89% — coming from payroll taxes. An additional 8% came from the taxation of Social Security benefits, while smaller sources of income came from general revenue and beneficiary premiums.
Most Medicare enrollees don't pay anything for Part A while they're enrolled in Medicare. For recipients over age 65, that's because of the Medicare taxes paid on income while working. Similarly, those who qualify for Medicare through a disability or medical condition also do not have to pay for Medicare Part A while enrolled.
How is Medicare Part B funded?
Nearly 75% of the $452.3 billion annual budget for Medicare Part B comes from general revenues, which are primarily raised through federal income taxes and other government taxes.
Another 25% of funding comes from the monthly premiums that Medicare Part B enrollees pay. Interest on Social Security payments accounts for a very small portion, less than 1%, of Part B funding.
The amount that Part B enrollees pay is adjusted annually. And in 2022, the standard monthly cost of Medicare Part B is $170.10, which is automatically deducted from Social Security payments. Enrollees with an income higher than $91,000 per year pay higher rates.
How is Medicare Advantage (Part C) funded?
Medicare pays private insurers administering Medicare Advantage plans a fixed amount every month for each beneficiary enrolled in their plans.
These funds are taken from Medicare Parts A and B treasury accounts to cover the costs of providing Medicare Parts A and B services under the policies. This usually amounts to more than $1,000 a month distributed to the insurance companies for each beneficiary enrolled in an Advantage plan.
In total, Medicare spends more than $348 billion on Medicare Part C funding each year. The program also pays plans an additional amount for providing drug coverage. In 2021, these funds covered more than 26 million beneficiaries enrolled in Medicare Advantage, which is 42% of the entire Medicare population.
The method for determining the costs of each beneficiary is based on a bidding process as well as a risk adjustment assessment that gauges the health of each beneficiary to better ascertain expenses.
Medicare Advantage plans submit bids that estimate the costs to insure each beneficiary, costs that are then compared to a benchmark rate that Medicare uses to determine health care costs in each county of the country.
If a plan or plans bid higher than the benchmark, beneficiaries pay the difference in the form of monthly premiums. If the plan or plans bid lower than the benchmark, the plan and Medicare split the difference between the bid and the benchmark rate. The plan’s share, known as a rebate, is then used to provide supplemental benefits to beneficiaries enrolled in the plan.
After the bidding process is complete, Medicare uses risk adjustments to gauge the health status of each beneficiary, and to thus modify the monthly fee to better reflect the cost of providing care to each beneficiary.
Like their counterparts in Original Medicare, Medicare Advantage beneficiaries are also required to pay monthly Medicare Part B premiums. Plus, there's the cost of the Medicare Part C plan, which averages $33 per month but could be $0 per month depending on the plan. Plans also charge deductibles and copays, bringing in additional revenues to pay for medical care.
How is Medicare Part D funded?
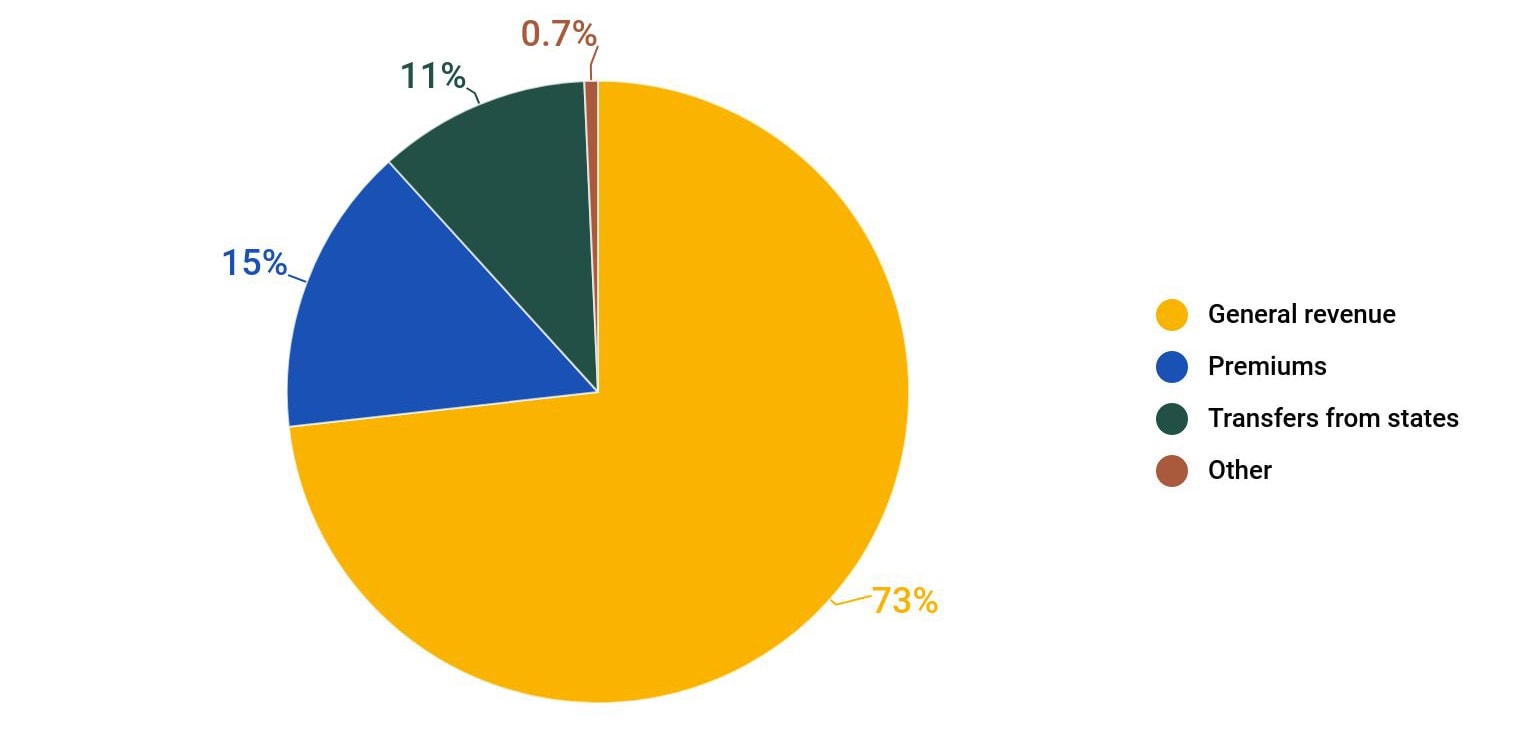
About 73% of the $105.8 billion in Medicare D spending is derived from general revenue. An additional 15% is generated by beneficiary premiums, while another 11% in funding comes from payments from the state for dual eligible beneficiaries who qualify for both Medicare and Medicaid because of having a low income.
Medicare Part D is an optional benefit that helps beneficiaries enrolled in Original Medicare pay for prescription drug coverage. Private insurance companies administer Part D prescription drug plans, charging beneficiaries premiums, deductibles and copays as part of the policies’ coverage of prescription drugs.
How are Medicare Supplement plans funded?
Unlike other parts of Medicare, supplemental plans are entirely supported by beneficiary premiums and coinsurance costs. The plans do not receive money from the federal government.
Because Medicare Parts A and B cover only about 80% of medical costs, a supplemental plan is used to fill in the coverage gaps and reduce the amount that enrollees pay for medical care. Beneficiaries buy supplemental plans, which are also known as Medigap policies, from insurance companies such as Aetna, Cigna and UnitedHealthcare.
What are the two treasury accounts used to pay for Medicare?
The federal government relies on two trust funds to finance Medicare services provided through Medicare Part A and Medicare Parts B and D, respectively.
One trust fund, known as the Hospital Insurance (HI) Trust Fund, supplies money for Part A services. The other trust fund, known as the Supplemental Insurance (SMI) Trust Fund, provides money for Parts B and D. In other words, Part A draws funding from the HI Trust Fund, while Medicare Parts B and D derive funding from the SMI Trust Fund.
The HI Trust Fund is funded through the following sources that finance Part A:
- Payroll taxes from employers and employees
- Part A premiums from people who don’t qualify for premium-free Part A
- Income from taxes from Social Security benefits
- Interest from trust fund investments
The SMI Trust Fund is funded through sources that provide money for Parts B and D:
- Funds authorized by Congress
- Beneficiary premiums
- Interest accrued from trust fund investments
Will Medicare funding run out?
Congress allocates money for the SMI Trust Fund based on estimated need each year, thereby averting any potential funding shortfalls. Unlike the SMI Trust Fund, the HI Trust Fund does not receive an annual appropriation from Congress, making the trust fund susceptible to economic conditions — downturns, for example, that diminish revenues from payroll taxes while health care costs and Medicare enrollments continue to increase.
As a result, Medicare Part A spending is outpacing Medicare Part A revenues, leading to a slow but sure depletion of funds.
In 2021, the Congressional Budget Office (CBO), predicted that the HI Trust Fund would run out of funds by 2026. The CBO predictions, like other predictions, are based, in large part, on economic forecasts.
When Medicare Part A has faced projected shortfalls in the past, Congress has stepped in to avert the deficits. The CBO estimates that a total of $517 billion in spending reductions, additional revenues or a combination of both will be needed to cover the difference between Part A spending and revenues from 2026 to 2031.
Frequently asked questions
Who pays for Medicare?
Medicare is funded through multiple sources: 46% comes from general federal revenue such as income taxes, 34% comes from Medicare payroll taxes and 15% comes from the monthly premiums paid by Medicare enrollees. Other sources of funding included taxation of Social Security benefits and earned interest.
Is Medicare funded by the state or federal government?
Medicare is a federal program, and as a result, the vast majority of Medicare funding comes from the federal government. However, state governments do make a small contribution for enrollees who qualify for both Medicare and Medicaid.
What percentage of Medicare is paid by the federal government?
The federal government finances 99% of the Medicare budget, while the remaining 1% comes from states.
Are Medicare and Medicaid funded in the same way?
Medicare and Medicaid are two different programs, serving two disparate populations, and the programs are funded differently. As a federal program, Medicare relies on the federal government for nearly all of its funding. Medicaid is a joint state and federal program that provides health care coverage to beneficiaries with very low incomes. It relies on both state and federal funds for financing.
How much does the government pay Medicare Advantage plans?
Medicare pays Medicare Advantage plans more than $1,000 a month for each beneficiary enrolled in their plan. Medicare spends more than $348 billion on Medicare Part C funding each year.
Sources
Information about Medicare funding is based on the 2021 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds that was released on Aug. 31, 2021, using data about the 2020 Medicare program. Additional sources include the Centers for Medicare & Medicaid Services (CMS) for Medicare cost data and the Congressional Budget Office (CBO) for fund projections.
ValuePenguin.com is owned and operated by LendingTree, LLC ("LendingTree"). All rights reserved.
Invitations for application for insurance may be made through QW Insurance Solutions, LLC ("QWIS"), a subsidiary of QuoteWizard.com, LLC ("QuoteWizard"), a LendingTree subsidiary, or through its designated agents, only where licensed and appointed. Licensing information for QWIS can be found here. QWIS is a non-government licensed health insurance agency. Not affiliated with or endorsed by any government agency.
Callers to QWIS will be directed to a licensed and certified representative of Medicare Supplement insurance and/or Medicare Advantage HMO, HMO SNP, PPO, PPO SNP and PFFS organizations. Calls to QWIS will be routed to a licensed agent who can provide you with further information about the insurance plans offered by one or more third-party partners of QWIS. Each of the organizations they represent has a Medicare contract. Enrollment in any plan depends on contract renewal.
Availability of benefits and plans varies by carrier and location and may be limited to certain times of the year unless you qualify for a Special Enrollment Period. QWIS does not offer every plan available in your area. Any information provided is limited to those plans offered in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Deductibles, copays, coinsurance, limitations, and exclusions may apply.
Medicare has neither reviewed nor endorsed the information contained on this website.
Editorial Note: The content of this article is based on the author’s opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.
