EPO Health Plans: What Are They?
Find Cheap Health Insurance in Your Area
An exclusive provider organization (EPO) insurance plan contracts with a network of doctors, hospitals and other health professionals to provide services to subscribers. An EPO allows for in-network specialty care without a referral but will not cover out-of-network services except in emergencies.
What is an EPO health plan and how does it work?
An exclusive provider organization (EPO) is a type of major medical insurance plan that provides minimum essential coverage for illness, hospitalization and preventive health care. As a managed care program, an EPO contracts with a network of primary care and other providers to deliver health services to members.
EPO insurance manages costs by limiting care to doctors, specialists and hospitals within the plan network. If you use an out-of-network provider, you are responsible for the full cost, except in emergencies.
While an EPO health plan requires using network providers, you don't need referrals for specialist visits. But you may need prior authorization. This means the EPO must review and approve the specialty visit first. Contact your insurance company or health care provider to ask about coverage.
EPO advantages:
- Mid-level premium costs: EPO premiums are generally higher than health maintenance organization (HMO) premiums but lower than preferred provider organization (PPO) rates.
- No PCP required: You do not need to select a primary care provider (PCP) to coordinate your health care needs.
- Access to specialty care: No specialist referrals are needed, but you must use in-network providers and may need prior authorization.
EPO disadvantages:
- Network limitations: Except in emergencies, you must receive care within the EPO network. You are responsible for the full cost of all out-of-network services.
- Other out-of-pocket costs: While EPO premiums may be lower, compared with other plan types, they may charge deductibles and coinsurance. HMO and point of service (POS) plans generally don't have deductibles.
EPO vs. other managed care plans: How are they different?
EPO health insurance and other managed care plans differ when it comes to provider selection, flexibility and cost. With EPO and HMO plans, you must get medical care within the plan's provider network. However, EPOs don't require referrals for specialty services as an HMO does.
PPO and POS plans allow you to go outside the network, but you may have to pay out-of-pocket fees such as deductibles, coinsurance or both. You may also pay a higher premium for network flexibility, compared with HMOs and EPOs.
EPO vs. other common health plan types
EPO | HMO | PPO | POS | |
|---|---|---|---|---|
| Average premium | Mid-level | Lower | Higher | Mid-level |
| Low or no deductible | — | ✓ | — | ✓ |
| Nonemergency out-of-network services covered | — | — | ✓ | ✓ |
| Specialist visits allowed without a referral | ✓ | — | ✓ | — |
EPO vs. HMO
EPOs require you to use network providers for routine care, similar to HMO plans. The main difference is that with an HMO, you must choose a PCP to coordinate your medical care and refer you for specialist visits. With an EPO, you can see specialists without a referral. You'll need to check that the provider is in your network, though, and whether you need prior authorization.
EPO vs. PPO
Like a PPO, an EPO does not require specialty referrals. But, while a PPO generally provides some coverage for out-of-network services, an EPO only covers in-network care, except in emergencies. Both EPOs and PPOs usually charge a deductible, which is the amount you pay out of pocket before coverage begins.
EPO vs. POS
POS health plans allow for care both in and out of network, but you'll pay more for out-of-network services. POS members must choose a PCP to manage care and provide specialist referrals. With an EPO, you're restricted to in-network care but do not need to select a PCP or obtain referrals. POS plans generally don't charge a deductible.
How much does an EPO cost?
EPO premiums are often on par with POS premiums, while HMO rates may be lower and PPO rates higher. In this chart, you'll find a comparison of rates for the four plan types using the average premium for a 40-year-old member.
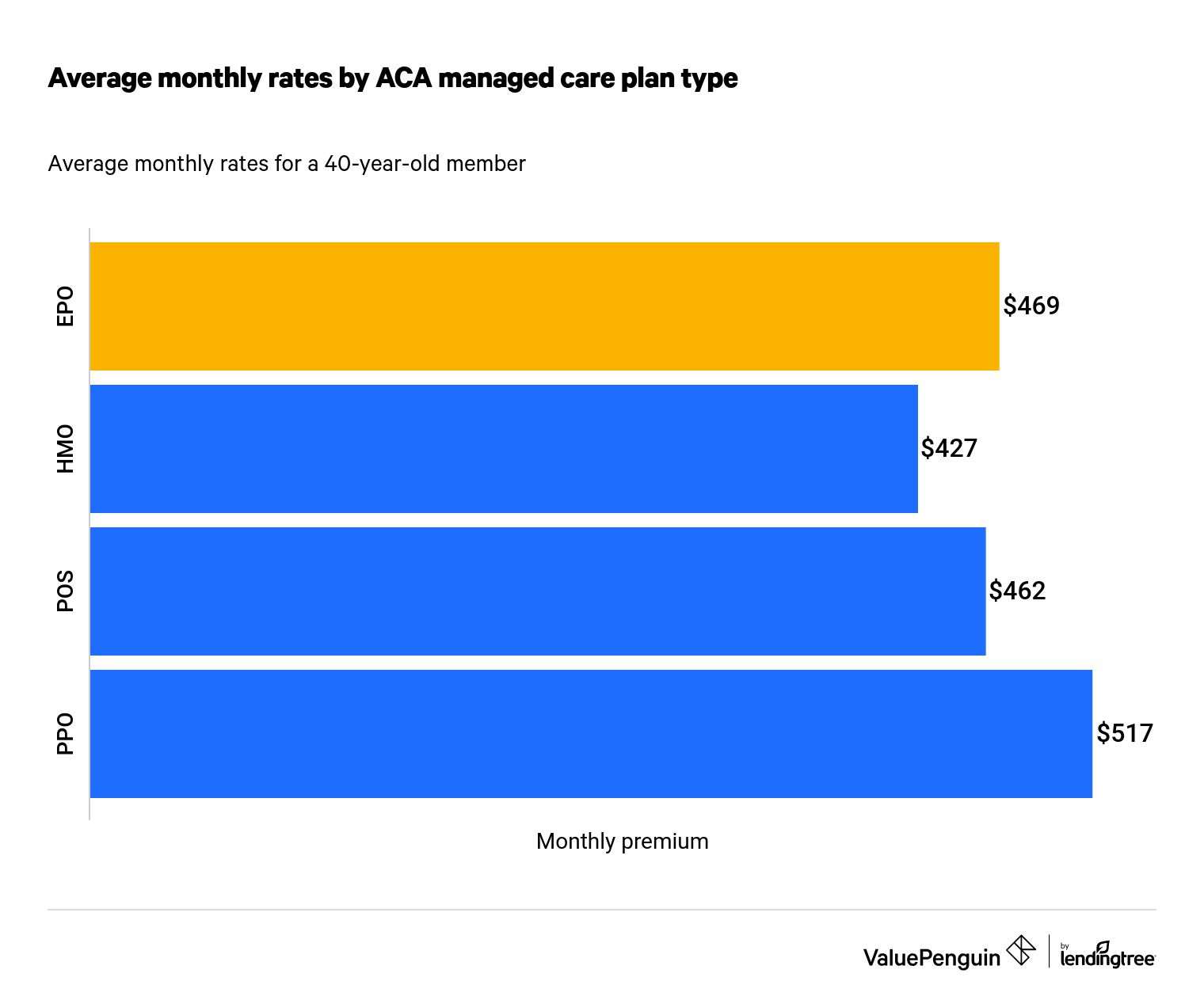
As you can see, EPO plans aren't the cheapest option. HMO plans have the lowest rates, partly because HMOs require referrals for specialty care — a practice that helps keep down overall costs. PPOs have the highest rates but offer the greatest flexibility, with partial out-of-network coverage and the ability to see a specialist without a referral.
Should I choose an EPO plan?
The choice between EPOs and other health plans often comes down to cost, choice and flexibility. An EPO is a middle ground, with medium rates and the ability to go directly to a specialist without a referral. However, the specialist must be in your plan's network.
HMO plans are the cheapest option with the least flexibility. If you have few health concerns and don't mind working with a PCP and staying in network, an HMO could be a good option.
PPOs allow for both in-network and out-of-network care, but you'll pay more out of network. Generally, PPO premiums are the highest of the four plan options.
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.
