What Is Medicare, and How Does It Work?
Find Cheap Medicare Plans in Your Area
Medicare is a federally funded insurance program that provides health coverage to seniors and those who have a disability or a qualifying medical condition.
The nationwide program helps pay health care costs for nearly 64 million people throughout the United States, helping about 56 million seniors and roughly 8 million disabled individuals pay for their health care.
What is Medicare?
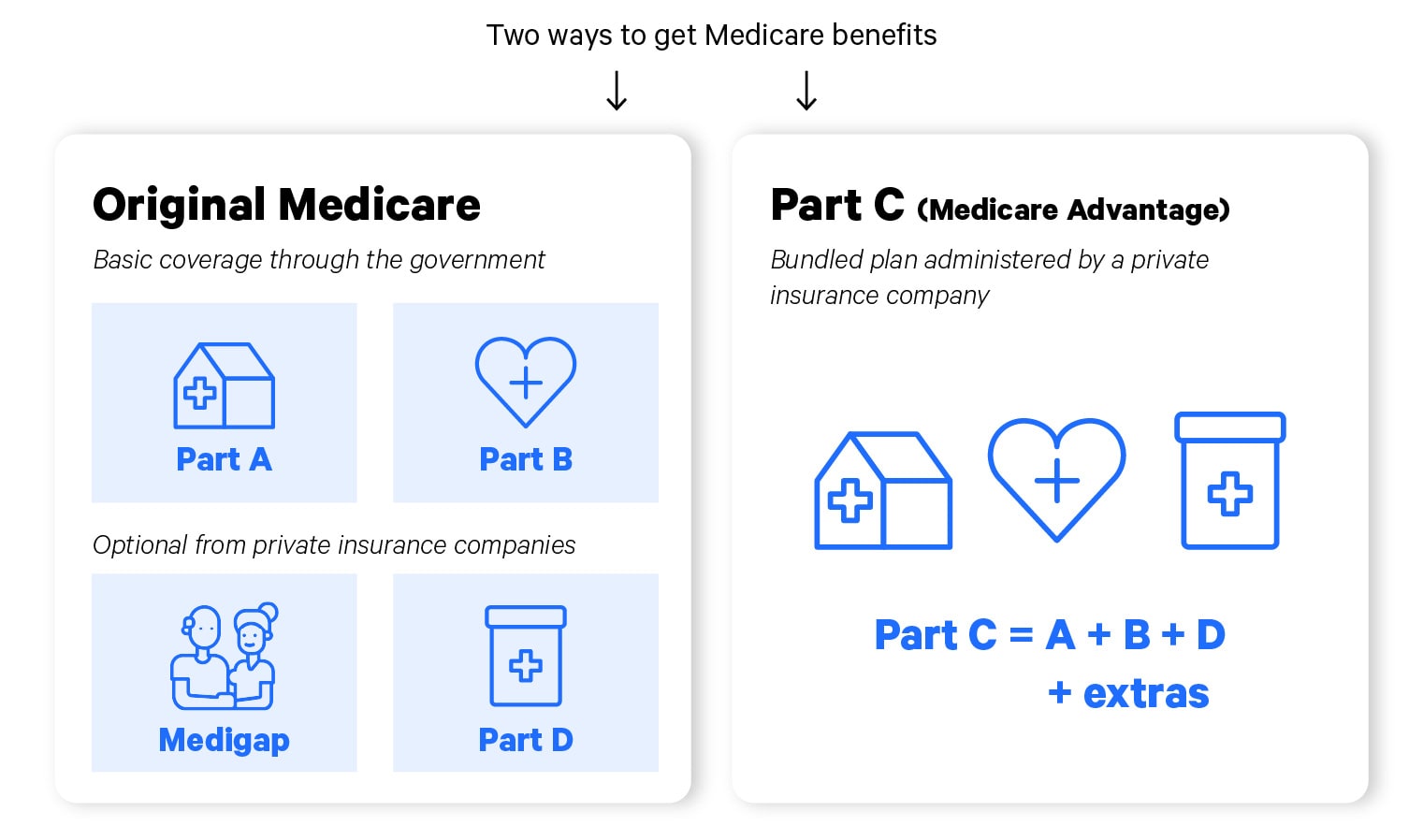
Medicare is a health insurance program that's divided into four separate and distinct parts — Parts A, B, C and D. Each part pertains to at least one specific area of coverage such as hospital care, doctor appointments or prescription drugs.
Medicare enrollees will typically choose either a bundled Medicare Advantage plan sold by a private insurance company or Original Medicare coverage through the government with optional add-ons from private insurers.
Medicare represents guaranteed health care coverage for those who qualify, regardless of income, health status or location in the United States.
The program is required to cover medically necessary care — essentially reasonable or necessary services intended to save lives while maintaining or enhancing care.
Moreover, the Medicare program is prohibited from charging you more based on your current or past health status. This is true whether you are enrolled in Original Medicare or Medicare Advantage.
Like other health insurance programs, Medicare requires you to meet deductibles, copays and coinsurance. In other words, Medicare is not a free program.
In some ways, it functions like an employer-based health care plan because you'll pay a monthly fee for coverage and a portion of health care costs.
Who is Medicare for, and when does coverage begin?
Ways to qualify for Medicare:
- Be 65 or older
- Have a qualifying disability
- Have end-stage renal disease
- Have Lou Gehrig’s disease (ALS)
Most people qualify for Medicare when they turn 65, making Medicare the primary source of health care coverage for millions of older Americans.
Coverage typically begins either the month you turn 65 or a few months after, depending on when you sign up. In some cases, you may be able to postpone your coverage if you’re still working past age 65.
You can also qualify for Medicare because of a disability or medical condition. This is generally defined as an illness or condition expected to last at least one year while depriving you of a certain amount of income each month.
For those who qualify because of a disability, Medicare typically goes into effect 24 months after you start receiving Social Security Disability Insurance (SSDI). However, the 24-month waiting period does not apply to permanent kidney failure, also called end-stage renal disease (ESRD), and amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease. With these two conditions, Medicare coverage begins as soon as you start receiving SSDI payments.
What are the parts of Medicare?
Original Medicare
Medicare Advantage
-
Medicare Part A: Covers inpatient care in a hospital or skilled nursing facility.
-
Medicare Part B: Covers outpatient services such as physician appointments, tests and treatment.
-
Medicare Part D: An optional prescription drug plan.
-
Medicare Supplement (Medigap): An optional plan to help reduce the medical costs left by Parts A and B.
Original Medicare
-
Medicare Part A: Covers inpatient care in a hospital or skilled nursing facility.
-
Medicare Part B: Covers outpatient services such as physician appointments, tests and treatment.
-
Medicare Part D: An optional prescription drug plan.
-
Medicare Supplement (Medigap): An optional plan to help reduce the medical costs left by Parts A and B.
Medicare Advantage
-
Medicare Advantage (Medicare Part C): Bundled insurance plans that include the services covered by Original Medicare (Parts A and B). Plans often include prescription coverage and extras such as dental or vision care.
The two components of Original Medicare, Parts A and B, are administered by the federal government, which delivers health care via fee-for-service arrangements by contracting with the 99% of medical providers throughout the country who accept Medicare.
With Medicare Advantage, coverage is administered by a private health insurance company that's operating as part of the Medicare program. These bundled plans are an alternative to Original Medicare. However, coverage, costs and provider networks vary by plan.
Medicare Part A
Medicare Part A covers inpatient care in a hospital or skilled nursing facility, but it does not cover custodial or long-term care.
What's covered by Part A?
- Inpatient hospital care
- Skilled nursing facility care
- Nursing home care
- Hospice care
- Home health care
What does Part A cost?
- Plan cost: Most enrollees do not have a monthly cost for Medicare Part A because they have worked and paid Medicare taxes on their income for at least 10 years. However, if you don’t qualify for premium-free Medicare, the cost of Part A can be up to $506 a month for 2023.
- Cost of care: You must meet a $1,600 deductible before Medicare Part A coverage kicks in and starts to pay for your inpatient care. After this, you don’t pay any medical costs for Part A services until day 61 of your hospitalization, when you'll pay a portion of medical costs called copays.
Learn more: Medicare Part A
Medicare Part B
Medicare Part B covers medically necessary doctor appointments, treatments and other outpatient services that don't involve a hospital stay.
What's covered by Part B?
- Doctor visits, medical tests and other outpatient care
- Outpatient hospital services
- Some home health services
- Durable medical equipment
- Therapeutic services
- Ambulance services
- Preventive services
- Chiropractic care
What does Part B cost?
- Plan cost: Medicare Part B has a standard monthly cost of $164.90 for 2023. There are higher monthly premiums for those with a high income. Those who have a low income can qualify for reduced costs through a Medicare Savings Program.
- Cost of medical care: Part B carries its own out-of-pocket costs, imposing a $226 annual deductible, the amount of medical care you have to pay for before coverage actually starts. After meeting your deductible, you’ll typically pay a 20% copayment for each medical service.
Learn more: Medicare Part B
Medicare Parts A and B do not cover the following services:
- Acupuncture
- Hearing aids
- Routine foot care
- Cosmetic surgery
Medicare Part D (prescription drug plans)
Medicare Parts A and B do not provide prescription drug coverage. But fortunately, beneficiaries enrolled in Original Medicare have the option of obtaining prescription drug coverage from Medicare Part D plans.
Private drug companies administer and sell Part D plans as part of the Medicare program. (Part D is not available to beneficiaries enrolled in Medicare Advantage since many of the Medicare Advantage plans provide prescription drug coverage.)
What does Part D cost?
- Plan cost: The cost of a Part D plan depends on the Part D policy you select. Monthly rates average $49.
- Cost of prescriptions: Plans come with different combinations of coverage and cost sharing. The maximum deductible for 2023 is $505, but your plan may charge less.
What prescriptions are covered?
Medicare Part D plans cover prescriptions across all drug categories, but the specific drugs may vary by plan. Medications are grouped into coverage tiers that affect how much you’ll pay for prescriptions:
- Tier 1: Generic prescription drugs (low copays)
- Tier 2: Preferred brand-name drugs (medium copays)
- Tier 3: Nonpreferred brand-name drugs (higher copays)
- Tier 4: Very expensive prescription drugs (highest copays)
Even though Part D is optional, if you enroll in Original Medicare you will probably need to enroll in Part D unless you have other prescription drug coverage such as a retiree plan through a former employer. Without a Part D plan or another form of creditable drug coverage, beneficiaries can easily spend thousands of dollars on brand-name medications, quickly outstripping many budgets.
Remember to enroll on time. There is a late penalty for not enrolling in a Part D plan during your initial enrollment period, which usually ends three months after you turn 65. The late penalty is a permanent amount added to your overall Medicare Part D premiums for as long as you have Medicare Part D coverage.
Learn more: Medicare Part D
Medicare Supplement (Medigap)
Medicare Supplement plans, also called Medigap plans, complement Original Medicare coverage by reducing or eliminating your portion of medical expenses after Medicare Parts A and B pay their share.
Medicare Parts A and B only cover about 80% of medical costs, leaving 20% for you to pay. And these costs can quickly add up, amounting to hefty bills if you only have Parts A and B. As a result, most beneficiaries enrolled in Original Medicare also enroll in Medigap to limit their medical expenses.
Private insurance companies administer and sell Medigap plans, which are labeled A through N. The letters denote the extent of coverage. In most cases, Original Medicare approves a claim and pays its share before sending the remainder of the bill to the Medigap policy.
What does Medigap cost?
- Cost of plans: The cost of Medigap plans varies widely based on factors such as where you live and the level of coverage you choose. The typical cost is around $165 per month, and requesting a quote is the best way to understand how much you might pay based on your situation.
-
Cost of medical care: Each Medigap plan has a standardized set of medical benefits, no matter what company you choose. The most popular options, Plans F and G, cover the most medical expenses including 100% of the copays for hospitalization, physician services and outpatient care. This could reduce your medical costs to a few hundred dollars per year or less.
There are no federal statutes requiring insurance companies to sell Medigap policies to people under 65 enrolled in Medicare. Therefore, availability varies by state.
Initial enrollment period is the best time to sign up for Medigap
Insurance companies cannot refuse to sell you a supplemental plan if you apply during your initial enrollment period, which occurs only once for most beneficiaries. For seniors, your initial enrollment period starts when your Part B coverage becomes effective and ends six months after that effective date.
If you fail to apply for a Medigap policy during your initial enrollment period, Medigap providers in most states can ask you health questions and then accept or decline your application or charge you more money based on your health status.
Learn more: How to compare Medicare Supplement plans
Find Cheap Medicare Plans in Your Area
Medicare Advantage (Part C)
Medicare Advantage, also called Medicare Part C, is a bundled health insurance plan that's sold and administered by a private insurance company as a part of its contract with the government.
What’s covered?
Medicare Advantage plans are required to cover the same services as Original Medicare's Parts A and B. This includes essential doctor care, hospitalization and medical treatment. Many plans also include Part D benefits for prescription drug coverage, as well as additional benefits such as hearing, dental and eye care.
What are the costs with Medicare Advantage?
- Original Medicare: Those enrolled in Medicare Advantage still must pay the cost of Original Medicare as a part of their participation in the Medicare program. This is typically $0 for Part A and $164.90 per month for Part B.
- Cost of the Medicare Advantage plan: The average cost of Medicare Advantage is $28 per month, but plans could be as cheap as $0 per month. There are also "giveback plans" that cost $0 per month and will reduce what you pay each month for Part B. These plans are widely advertised by insurance companies, but they have very limited availability.
- Cost of medical care: How much you pay for health services varies by plan and is determined solely by the coverage of the plan in which you enroll. The standardized cost-sharing rules of Original Medicare are replaced by your Medicare Advantage plan's deductible, copays and out-of-pocket maximum.
What are the types of Medicare Advantage plans?
Medicare Advantage plans rely on provider networks to provide care, usually employing health maintenance organizations (HMOs) and preferred provider organizations (PPOs) to deliver that care.
- With HMOs, you are required to obtain care from the plan’s network of providers except in emergencies. You are also required to choose a primary care physician who is responsible for managing your overall health care, referring you to specialists, for example.
- PPOs give you more flexibility than HMOs — you don’t have to choose a primary care physician to manage your care, for example, and you don’t have to obtain prior approval to see a specialist. With many of the PPOs, you can also go outside of your network of doctors, but this will cost you more money.
Is Medicare Advantage right for you?
When choosing between Original Medicare and Medicare Advantage, you have to determine what you want and value in a health plan. For example, if you want a plan with more freedom of choice in picking a provider, Original Medicare is a better fit. If you want a plan with more included perks, Medicare Advantage is a better fit.
What's good about Medicare Advantage:
- Plans are simpler in many ways because care and services are contained in one plan. In contrast, Original Medicare enrollees are required to purchase prescription drug coverage and supplemental coverage separately.
- Plans have extra benefits, and some plans also cover gym memberships, preventive chiropractic care and stipends for over-the-counter supplements.
- Plans have yearly caps on out-of-pocket expenses that cannot exceed more than $8,300 a year for in-network care. This is especially good for those who have ongoing medical conditions because if you have Parts A and B alone under Original Medicare, you don’t have a cap on your medical spending, meaning there is no limit to what you could spend out of pocket.
What's bad about Medicare Advantage:
- There are restrictions on medical providers: Medicare Advantage, unlike Original Medicare, has financial incentives or outright stipulations requiring you to access care from network providers except in emergencies.
- Plans have geographic limitations: Beneficiaries can only enroll in plans offered in their ZIP code, and networks of medical providers often have a regional service area. This is different from Original Medicare where beneficiaries can access care from over a million providers in the country.
- Your costs are dependent on the amount of medical care you need: Many beneficiaries assume Medicare Advantage plans are cheaper alternatives because their monthly premiums are often low or even nonexistent. But most of the costs with Medicare Advantage plans come from copays, coinsurance, deductibles and other medical costs that emerge as part of the overall care process. If you need expensive medical care, you could end up paying more under Medicare Advantage than you would with Original Medicare.
- Plans can require preauthorization: Your insurer may need to approve some tests and treatments before you'll have coverage. A study on Medicare Advantage prior authorizations found that plans wrongly denied an estimated 85,000 medical requests in 2019, indicating some of the problems you could have with coverage.
Learn more: What are the best Medicare Advantage plans?
Medicare enrollment periods
Medicare, like many types of insurance, has enrollment periods: an initial enrollment period, a special enrollment period, a general enrollment period and an open enrollment period.
Medicare's initial enrollment period is the seven-month window around your 65th birthday — starting three months before your birthday month, running through your birthday month and ending three months after your birthday month.
Most experts recommend that you apply for Medicare three months before your 65th birthday so you have Medicare coverage by the time you turn 65.
If you are receiving Social Security benefits prior to age 65, Medicare assumes you are retired and need Medicare benefits. In this case, Medicare automatically signs you up for the government program and sends your Medicare card in the mail. You will still need to manually enroll in your choice of Medicare Advantage, Medicare Part D or Medigap plans.
If you have no other coverage and fail to enroll in Medicare during your initial enrollment period, you will have to pay a late enrollment penalty. However, you may be able to defer enrollment in the parts of Medicare that have a monthly cost if you are working and receiving health care benefits from a company with more than 20 employees.
The general enrollment period runs from Jan. 1 to March 31 each year, giving people a chance to enroll in Medicare if they missed their initial enrollment period. For most people, this is the only time they can enroll in Medicare if they did not sign up when they first became eligible. Some people may have to pay a late penalty depending on their circumstances. Coverage starts on the first of the following month after you enroll in Medicare during a general enrollment period.
With a special enrollment period, you can make changes to your Medicare Advantage plan or your Medicare Part D prescription drug coverage when a qualifying life event happens. This could occur in situations such as losing other insurance coverage or moving.
Enrollment time periods vary based on the qualifying event.
Let’s say, for example, that you did not sign up for Medicare because you have credible employer-based health coverage. If you lose this coverage, you'll qualify for an eight-month special enrollment period.
In another case, if you move out of a Medicare Advantage plan’s geographic area, you could qualify for a special enrollment period that allows you to enroll in another Advantage plan in your new location.
- Switch from Original Medicare to Medicare Advantage or vice versa
- Change Medicare Advantage plans
- Enroll in a Medicare Part D plan
- Change Medicare Part D plans
Frequently asked questions
What is Medicare insurance?
Medicare is a federally funded, national program that helps about 56 million seniors and roughly 8 million disabled individuals pay for their health care.
Is Medicare free?
Medicare is not a free program. Medicare enrollees are required to meet deductibles, copays and coinsurance, making the program similar to employer-based health care plans in this respect. Most enrollees typically pay between $165 and $350 per month for the components of Medicare.
Who qualifies for Medicare benefits?
Seniors 65 and older qualify for Medicare benefits, and individuals with certain health conditions and disabilities qualify for the program.
When can you sign up for a Medicare plan?
People who are close to turning 65 can enroll in Medicare during an initial enrollment period that starts three months before their 65th birthday and ends three months after their birthday month.
Does Medicare cover you if you’re traveling outside of the U.S.?
In most cases, Medicare will not pay for health care or supplies you obtain outside of the U.S. There are, however, exceptions. For example, Medicare will cover services in a foreign hospital if you suffer a medical emergency in the United States and the foreign hospital is closer than the American hospital.
Sources
- Medicare.gov
- U.S. Department of Health and Human Services
- Centers for Medicare & Medicaid Services
ValuePenguin.com is owned and operated by LendingTree, LLC ("LendingTree"). All rights reserved.
Invitations for application for insurance may be made through QW Insurance Solutions, LLC ("QWIS"), a subsidiary of QuoteWizard.com, LLC ("QuoteWizard"), a LendingTree subsidiary, or through its designated agents, only where licensed and appointed. Licensing information for QWIS can be found here. QWIS is a non-government licensed health insurance agency. Not affiliated with or endorsed by any government agency.
Callers to QWIS will be directed to a licensed and certified representative of Medicare Supplement insurance and/or Medicare Advantage HMO, HMO SNP, PPO, PPO SNP and PFFS organizations. Calls to QWIS will be routed to a licensed agent who can provide you with further information about the insurance plans offered by one or more third-party partners of QWIS. Each of the organizations they represent has a Medicare contract. Enrollment in any plan depends on contract renewal.
Availability of benefits and plans varies by carrier and location and may be limited to certain times of the year unless you qualify for a Special Enrollment Period. QWIS does not offer every plan available in your area. Any information provided is limited to those plans offered in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Deductibles, copays, coinsurance, limitations, and exclusions may apply.
Medicare has neither reviewed nor endorsed the information contained on this website.
Editorial Note: The content of this article is based on the author’s opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.
