Health Insurance
61% of Americans Have Been Surprised by an Unexpected Medical Bill — and 37% Pay Without Question

If the cost of treatment ultimately falls on unsuspecting consumers, it wouldn't be a new experience for most — but it would be financially difficult. In a recent survey by ValuePenguin, 61% of Americans reported receiving an unexpected medical bill at least once before, while 3 in 4 said that receiving an unexpected bill now would have significant financial consequences.
Key Findings:
- 61% of all Americans and 76% of parents with young children have experienced receiving an unexpected medical bill in the past.
- Almost 3 in 4 Americans agreed that they would be "significantly set back financially" if they received an unexpected medical bill today.
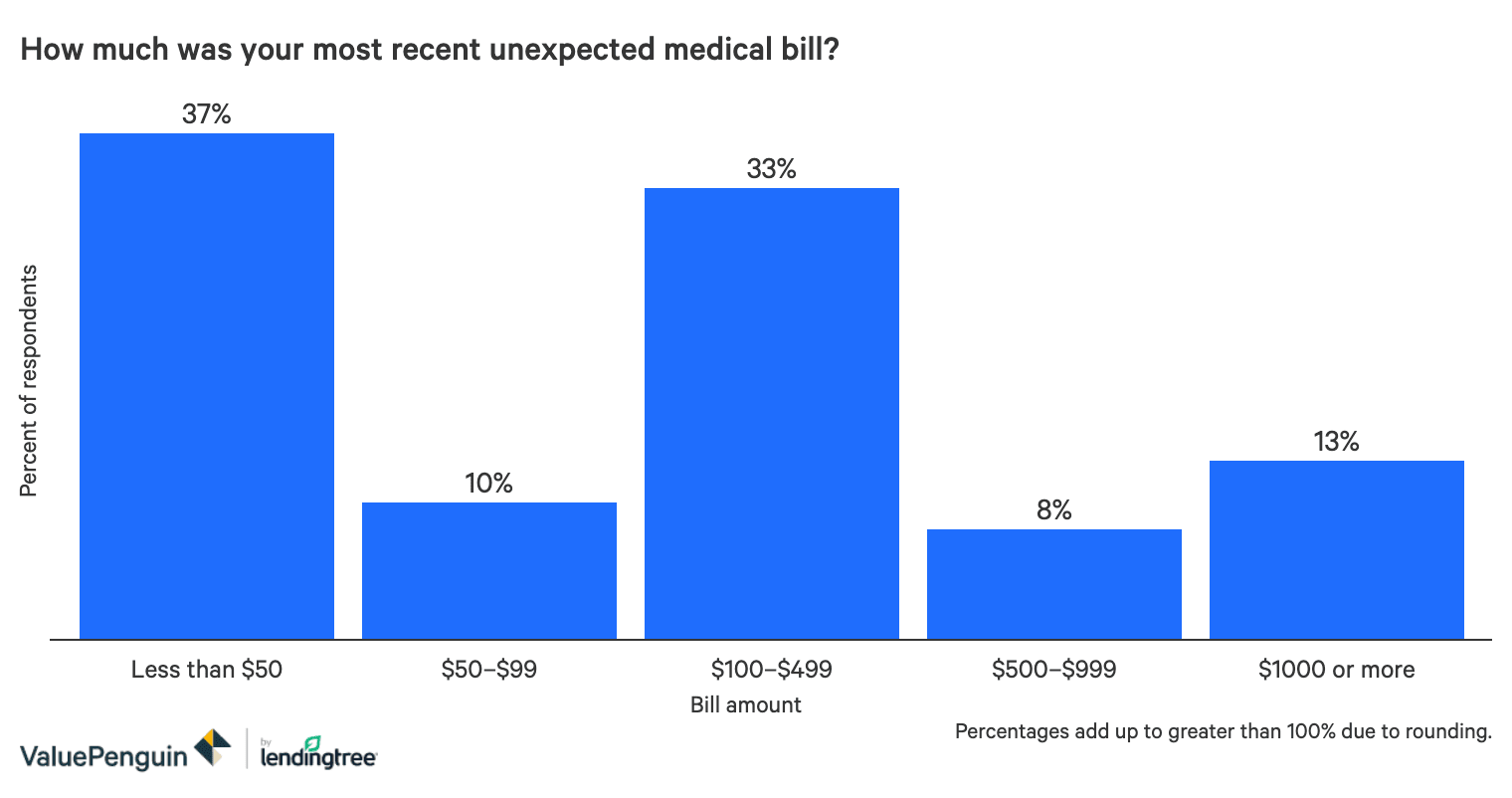
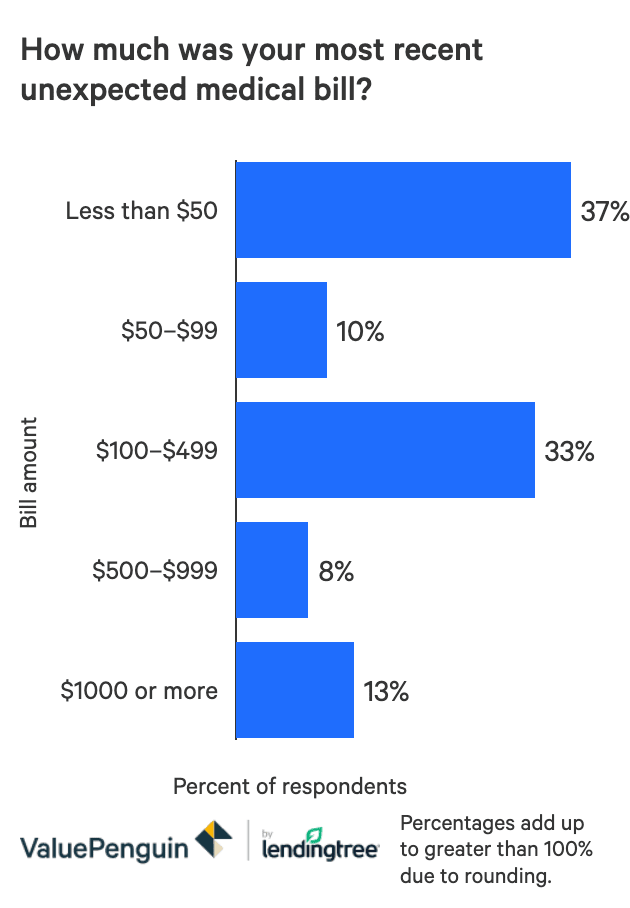
- On average, consumers’ most recent surprise medical bill totaled $520. The average woman’s bill was nearly $400 more than that of the average male.
- The most common unexpected charges included emergency room visits, health-related tests and specialist visits.
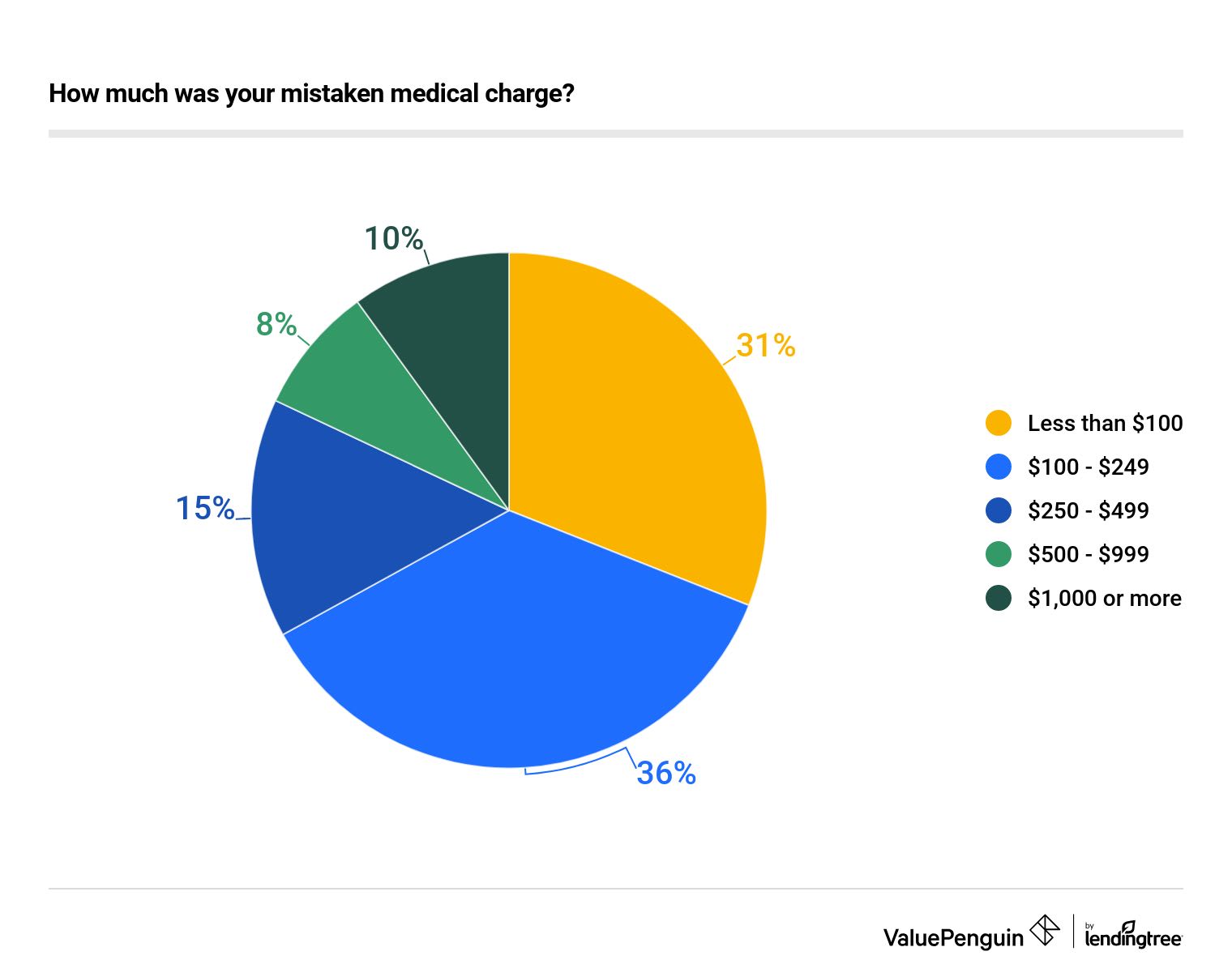
- Not many review their bills despite the benefits: 3 in 4 people don't review line items in each medical bill they get, even though 37% said that they have caught a mistaken charge before.
Overall, the survey results indicate that while a majority of Americans have prior experience with unexpected medical costs, neither their habits nor their finances are well-prepared to cope with the challenges of a surprise hospital bill due to COVID-19.
Most people have received an unexpected medical bill before, but even more say receiving one now would be a financial problem
Widespread experience with surprise bills hasn't led to more financial preparedness. Even though 61% of Americans have received an unexpected medical bill at some point, and 54% say they've received one in the last year, an even greater proportion (75%) admitted that receiving one now would "significantly" set back their finances.
Among respondents who had received one, the typical bill was about $520, though past bills ranged significantly across groups. Among women, the average bill total was $725, while men tended to pay much less; their typical bill was a comparatively scant $329.
Most commonly, the unexpected bill was for an expense they thought their insurer would cover (43%), with 18% being charged more than they expected and 6% billed for a treatment they didn't receive.
Emergency room visits and health tests are the most common unexpected charges
While respondents cited all types of medical needs as causes for their unexpected bills, emergency room visits and diagnostic tests were the most commonly cited among people we surveyed — they were each cited by 28% of respondents.
Visits with specialists rounded out the top three, with 23% of respondents surprised by the cost of these visits.
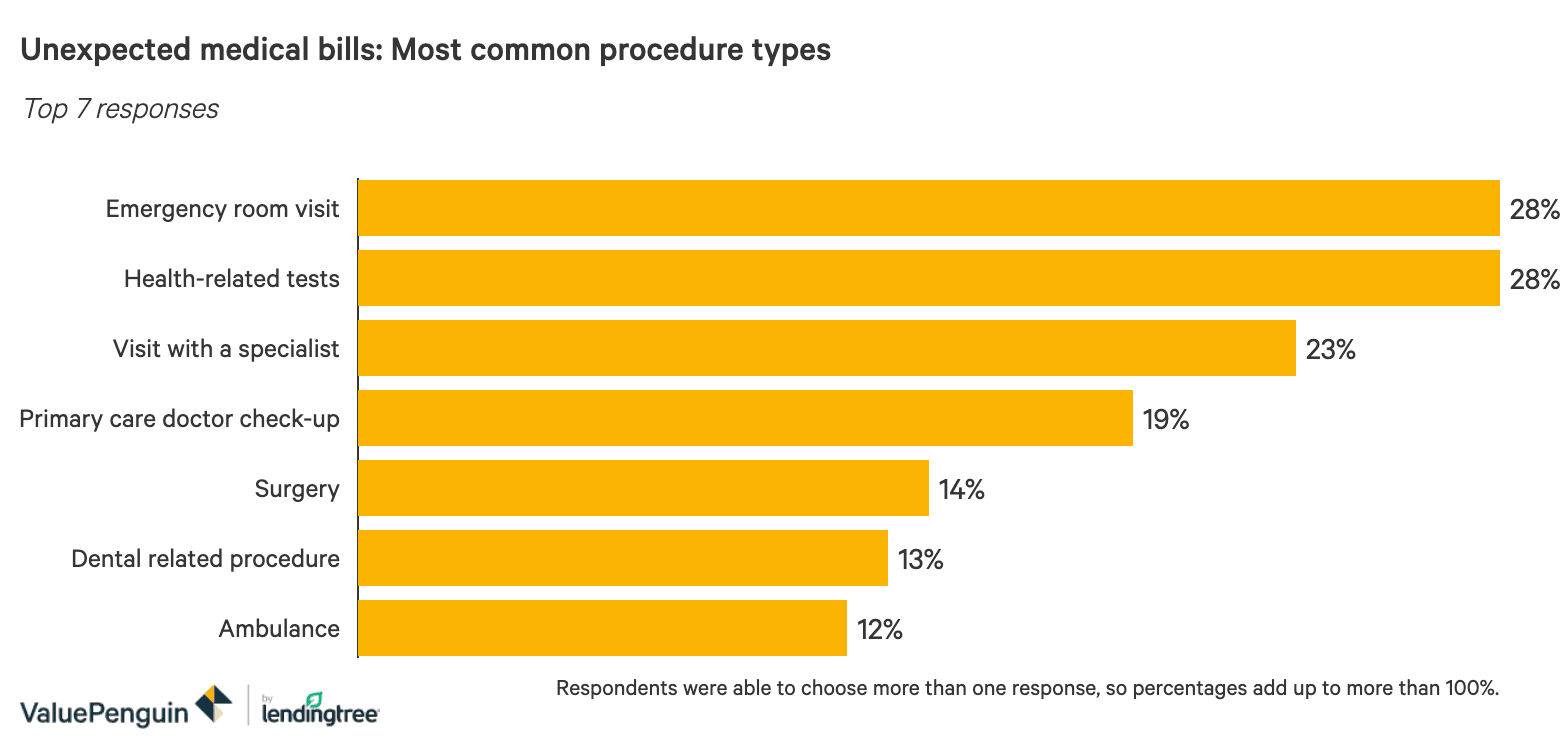

Despite the high, unpredictable cost of riding in an ambulance, relatively few respondents called that out as a major unexpected expense — only 12% did so.
The Families First Coronavirus Response Act was signed on March 18, guaranteeing free coronavirus testing for all Americans. However, for people who test positive, the test may only make up a small portion of the overall cost for people with serious cases; as of now, it's up to citizens and their health insurance to cover the rest of the bill.
Mistaken charges are common, but most people rarely review their bills
Our respondents suggested that errors in their medical bills are quite common. A full 37% said they'd found an error in at least one medical bill. And that's despite the fact that 44% of Americans "rarely" or "never" review the line-item expenses when paying a medical bill.
Younger Americans were less likely to review medical bills in detail. For instance, millennials are about half as likely as baby boomers are to say they "always" review items on their medical bills.
While the majority of errors amounted to under $250, some errors were far more: 23% of the mistakes amounted to between $250 and $1,000, with 11% going beyond $1,000.
Americans are torn over whether to inquire about the bill, or 'just pay it'
When confronted with an unexpected medical bill, the most common response was to simply pay it (37%). Among that group, nearly half didn't know they had any other options.
Other groups took a variety of actions in response to their surprise bills: 35% of people called to ask about the bill, and 15% appealed. Ten percent of respondents simply ignored it altogether.
We found a substantial difference in the habits of men and women when confronted with these bills. Women were most likely to call and ask about the bill (40%), while men were most likely to simply pay (47%).
What should you do if you receive an unexpected medical bill?
If you receive a medical bill you weren't expecting or can't understand, the first step should always be to gather more information by reviewing the line items, then calling your doctor's office or hospital if you need more information.
Ask the hospital to match the line items on the bill to the services or medications you actually received. For instance, you have been charged a full night's hospital stay even though you checked out in the evening. Line items for treatment might be duplicated or mixed up with more expensive versions of the treatment.
What to do when you have surprise medical bills
- Make sure you understand and have received every item.
- Ask your insurer — and your doctor — to double-check the line items in the bill.
- Negotiate a discount or payment plan.
- Ask for help from a patient advocacy group.
Make sure that your health insurance company has been kept in the loop on the charges. The bill may indicate that your insurance has not yet paid its due portion of the expenses, so your out-of-pocket costs might be lower than the number you see.
Resolving the matter may be as simple as having the doctor's office and your insurance company review the charges to ensure they didn't make any errors.
You can also ask for outside help. The Patient Advocate Foundation and other nonprofit or government groups may help you reduce the amount you owe, especially if you're paying for the procedure out of pocket.
If your health insurance has already covered the appropriate amount and you're still left with a difficult bill to pay, don't hesitate to negotiate a payment plan with the hospital. Most billing departments will offer at least some cooperation in breaking a big bill into manageable installments.
Methodology
ValuePenguin conducted an online survey of 1,311 Americans, with the sample base proportioned to represent the overall population. The survey was fielded using Qualtrics, Feb. 27-March 4, 2020.
